Last Updated on April 21, 2024 by Art
An Advantage to Children & Young Adults?

This is a timely and important question for all of us. Schools are re-opening for in-person teaching, offering more opportunities for coronavirus to spread. College students are partying in violation of campus orders, leading to increasing numbers of virus cases. And whatever happens to young people will be spread through their families to the entire population.
Today’s blog unpacks the latest research to address some nagging questions:
- Why do people under 25 practically never die from COVID?
- How worried should we be about kids returning to classrooms? It’s well known that classrooms help spread childhood diseases.
- College students are partying and getting infected. So why aren’t we all dead yet?
If you’re looking for the “aha!” moment, the ultimate answer, this blog may disappoint you. Because these questions are not yet completely settled. But I can give you today’s best answers.
Here are quick links to the main sections of this blog:
COVID-19 Youth: Reactions to Infection
Hospitalization & Mortality Data Favors COVID-19 Youth
COVID-19 Youth Infecting Others
COVID-19 Youth Immunity, Explained
COVID-19 Youth: Reactions to Infection
What do we know about COVID-19 youth responses? And what do we not know? By “youth” I mean people under age 25, that is, children and young adults.
– Excess Deaths Show That COVID-19 Youth Rarely Die
In a recent blog we reviewed Excess Deaths data, the truest, most objective measure of coronavirus infection. It neither over-estimates nor under-estimates the effect of this disease, and is relatively immune to misinterpretation. And one section of that blog discusses deaths by age group.
What does that data show about COVID-19 youth immunity, or near-immunity?
Simply this:
- The normal death rate of people over 65 increases about 40% in the presence of coronavirus.
- For people aged 25 to 64, their normal death rate increases by about 30%.
- However, for those under 25, their already very low death rate is increased by only 4.4%.
The data for the youngest age group is so dramatically different that it cries out for an explanation. And that explanation is forthcoming, so please keep reading!
– Coronavirus Is Not Yet On the Way Out
Note that the analysis above treated the weeks of highest excess death count in April and May. Why? Because the peak deaths at that time provided more data, allowing a more accurate analysis of how age affects COVID mortality.
However, now we’re past that peak. Therefore, is the coronavirus going away? Yes, and No:
Nationally, following the peak in April, we had another peak around the beginning of August. Since then, good news! Total excess US deaths have been declining.
However, individual states still have serious problems as of a September 30 report:
- 26 states exceed 12 new coronavirus cases per day per 100,000 population, more than three times the goal of healthcare experts.
- 30 states have an effective Reproduction number above 1, meaning that the virus is spreading rather than dying out.
- 33 states have a higher than 5% positive rate on coronavirus tests given, showing that they are not testing enough people to track and control the disease.
What is happening is that the high-population states that were hit first made good progress in controlling the virus, and that pushed down the nation-wide total death count. And now the virus is spreading in the less-populous states that initially escaped it.
We Americans travel a great deal state to state. Therefore, we should not count the virus as defeated so long as any states continue to be hot spots.
Hospitalization & Mortality Data Favors COVID-19 Youth
Excess deaths give the clearest, least arguable, data. However, there’s other data that speaks to COVID-19 youth immunity, if it exists. And that is the proportion of people hospitalized with coronavirus who die rather than get well.
CDC presents a dramatic and scary chart that analyzes how age affects your chance of going to the hospital and of dying:

Study the Hospitalization and Death rows on this chart and you will either heave a sigh of relief or gasp in panic. K through 12 kids are fabulously safer than the young-adult comparison group. On the other hand, the oldest groups are ten times more likely to enter the hospital, and hundreds of times more likely to die!
– Death Rate per Hospitalization
When I saw the CDC chart it made me ask, OK, if someone enters the hospital, what is their chance of death? And I soon discovered that this number is very squishy and difficult-to-interpret.
On August 24 StatNews published a study by Rothman et al to determine whether COVID-19 is becoming less lethal. The authors concluded that approximately 0.65% of people who contract coronavirus die, and that this percentage has not changed at all during 2020.
They then looked at the ratio of deaths to hospitalizations and derived the following chart:
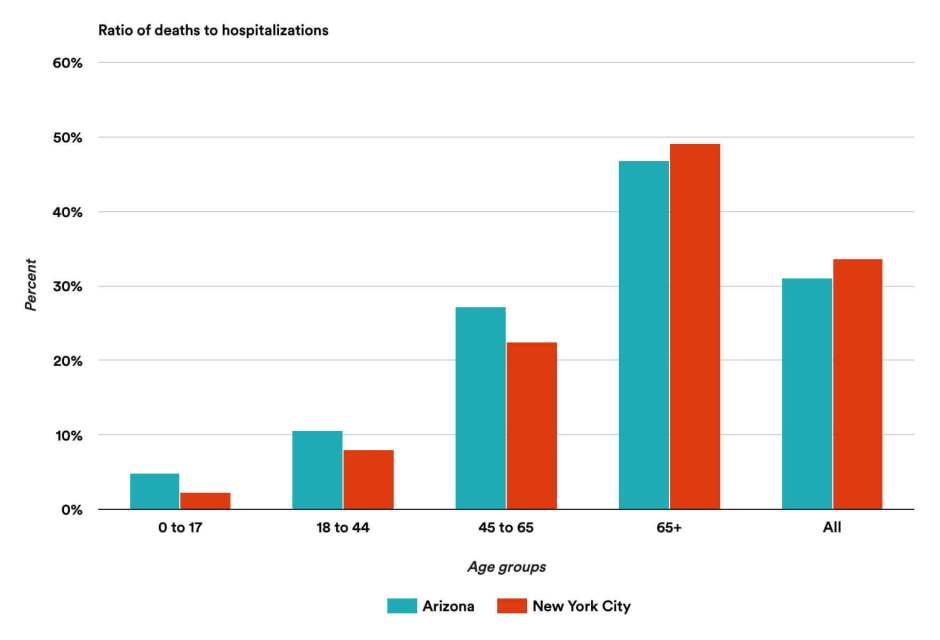
You might look at this chart and say, Huh? Why Arizona and New York City?
The authors explain that most states do not report both deaths and hospitalizations, so that the data simply isn’t available. However, Arizona and NYC have good data collection, and are two completely different venues: an early, crowded, high-fatality large city, versus a lower-density state that has only recently seen much COVID-19.
What can we learn from this chart?
- For these two locations the data are remarkably the same, not only the totals but also in every age group.
- We already know that fewer young people have to go to the hospital; this chart shows that when they go, they have a very high chance of survival.
- The death percentages are IMMENSE! Fifty percent of seniors going into the hospital with coronavirus die. WHAT?
This last number raises questions of its own, which I will now address.
– Art Explains Huge Hospital Death Rates
On October 2, the US had the unfortunate chance to hear doctors describe the probability that the President, a 74-year old man who had just entered the hospital with COVID-19, would survive the disease:
- Dr Zeke Emanuel, professor at University of Pennsylvania School of Medicine, stated that such a person’s chance of death would be between 5% and 11 or 12%.
- Dr Jon LaPook, a Professor of Medicine at NYU who is chief medical correspondent for CBS news, estimated the chance of death at 15%.
- And Dr Sanjay Gupta, an associate professor of neurosurgery at Emory University and chief medical correspondent for CNN, estimated the odds of survival at “90 to 95 percent,” which implies a chance of death between 5% and 10%.
These 5% to 15% numbers are scary for sure, but far less so than the 50% shown in the StatNews study. What is going on?
Here is my explanation: The patients described by the Arizona-NYC data did not enter the hospital until their coronavirus infection was seriously advanced. However, the doctors on the news are describing a different situation: the case of a man hospitalized with coronavirus early in the disease, “out of an abundance of caution.” They have not examined the patient and have only the very limited information that was made public. Therefore, they are giving their best guess based on what they know.
So I say to you, be very careful about projecting probability of death, just because someone went to the hospital. It could be very high or very low depending on many factors, including how soon they were admitted after learning that they were infected.
– Note added after publication
Prof. Rothman sent me an e-mail saying that he agrees with the above analysis. He then states: “What the Arizona numbers show is that people are still not getting to the hospital soon enough, despite all we have learned about the disease, and this probably still is the main determinant of the fatality rate, especially among the elderly.” I will add: if you start having symptoms, don’t delay seeing your doctor!
COVID-19 Youth Infecting Others

OK, so young people who catch coronavirus have very little chance of dying. (Although, even mild cases are subject to “sequelae” such as heart problems.) However, how infectious are they, both with other young people and with adults?
Here the data is confusing and contradictory. An LA Times article tried to pull some of it together:
- A study in India involved huge numbers of people: half a million tests of people who had come into contact with 84,000 confirmed coronavirus cases. Researchers found that although children younger than 17 were the least likely to die of COVID-19, they transmitted the virus at rates similar to the rest of the population. In addition, children ages 5 to 17 passed the virus to 18% of close contacts their own age.
- Chinese researchers studied 195 unrelated clusters of cases and over 2,000 of their close contacts. Children under 20 years were less than 30% as likely to become infected as adults over 60.
- In Iceland, a study of over 9,000 people showed that children under 10 years had only one-half the incidence of infection of all other age groups.
- Government guidance in the Netherlands advised that coronavirus is mainly spread between adults and from adult family members to children. The spread of COVID-19 among children or from children to adults is less common. In general, the younger the children, the less significant the role they play in spreading the virus.
In general, it seems that children are less likely to get infected. And when they are infected, the infections are milder and less likely to lead to death. However, there is disagreement as to whether children play a significant role in the spread of the virus through the general population. The conflicting results may depend upon national differences in family composition and behavior.
– Infection Spreads Through Super-Spreading Events

In a previous discussion of Herd Immunity we pointed out that a simple analysis of herd immunity assumes that everyone is equally susceptible, and contacts everyone else randomly. Which of course is not true in the real world.
A thoughtful article in Atlantic points out that there are two kinds of disease spread:
- Deterministic, in which a disease spreads in a steady manner, so that we can predict its course.
- Stochastic (chaotic), in which a very few “super-spreader events” are responsible for most of the infections. Whether or not they occur is random, the luck of the dice.
Researchers have found that coronavirus spreads stochastically. It seems to follow the Pareto Principle, also known as the 80/20 Rule: that for many events, only 20% of the causes lead to 80% of the results.
Amazingly, a Hong Kong study found almost exactly these percentages. Researchers traced contacts for more than 1,000 COVID-19 infections and found that 19% of the cases led to 80% of the secondary infections.
This exact match is accidental. More generally, studies of clusters suggest that 10 to 20% of the cases lead to 80 or 90% of the infections. And those infections occur most often at super-spreader events.
Based on my reading, super-spreader events may happen when you have a highly infectious person plus one or more of the following:
- Close contact, such as occurs with crowding
- Extended time being together
- Poor ventilation
- Loud talking, shouting or singing
- Not wearing a face mask
Of course, asymptomatic people can be infectious. You can’t tell if they are infected, nor can they. Do you want to be cautious? Then always assume that if someone you don’t live with is present, they may be the seed for a super-spreader event.
COVID-19 Youth Immunity, Explained
With all this confusing information, and the randomness of COVID-19 spread, it’s forgivable to throw up our hands and say, we just don’t know what the story is with young people. But recent research has discovered the “secret sauce” that protects people under 25 so well.
Human beings have two types of immune system:
- We are born with a primitive response to invasion, the innate immune system. Babies have millions of T cells with a huge variety of different receptors to recognize pathogens. They need them because every infection that a baby encounters is new to the baby. The innate immune system is very efficient at recognizing every kind of invader and immediately attacking it.
- As we get older, we start encountering the same viruses and bacteria over and over again. Our body finds it more efficient to reduce its variety of T cells and instead make additional copies (“memory T cells“) of the ones we may need to use again. Thus when we encounter a familiar disease, say the flu, our body can respond very quickly to defeat it. This evolved mature immune response is known as the adaptive immune system.
The problem is that coronavirus is a new disease, and our adult adaptive immune systems cannot recognize it and fight it. We need the flexible, fast-responding resources of our innate immune system, but unfortunately those withered away as we got older. For this reason, the younger a person is, the better they are able to suppress the COVID-19 virus, and recover from infection.
– COVID-19 Youth Immunity Is More Than A Theory

This neat explanation is more than guesswork. A group of medical researchers at Yale and Albert Einstein College of Medicine studied the immune system response of 125 patients with COVID-19. 65 were under 24 years of age, with average age of 13 ± 6; the other 60 were much older, with average age 61 ± 13.
The researchers found that two immune factors were very strong in the youths: interleukin 17A (IL-17A), which helps mobilize immune system response during early infection, and interferon gamma (INF-g), which combats viral replication. Both of them declined inversely with age.
The adults were not lacking in immune system response. On the contrary, their antibodies increased with the patient’s age, and they showed more vigorous T cell response to the virus. The problem appeared to be that the adult immune response was too slow. The youth were protected by a very rapid response, which inhibited the virus long enough that the body could mount defenses against it.
The higher antibodies present in adults can make the disease worse, which is called antibody-dependent enhancement. Most vaccine candidates boost antibody levels, and if they boost the wrong antibodies they could hurt rather than help the patient. Vaccine developers are being alert, hoping to avoid this problem. In contrast, however, the Yale researchers suggest that a vaccine that bolsters the innate immune response might be safer than the vaccines that raise antibody levels.
Answers and Conclusions
In conclusion, here’s what the above research has told us about COVID-19 youth immunity and the questions that we started with:
– Randomness
COVID is not deterministic, it’s random. A few people cause almost all of the cases, usually in crowded indoor venues. If you avoid those venues, and don’t work in healthcare, you are much less likely to catch the virus. But “much less likely” doesn’t mean “never,” it’s still a gamble.
– Youth Immunity
Young people are genuinely protected by the innate immune system they were born with and still have. This gives them an immunity to unfamiliar diseases which disappears as they get older.
– K through 12
What about kids returning to K through 12 classrooms? They will catch and spread COVID-19. Because they are somewhat immune, they will have a milder disease and (usually) not die from it. And a milder case is often less infectious. However, a kid can still give the virus to family members, who being older may suffer a more dangerous infection.
How do we reduce K-12 infections and spreading? Get your school to freshen the air! Masks and distance are not enough if the same air continuously circulates. Other possibilities: teach in pods (small groups), teach remotely, or reduce exposure with a mixture of virtual days and in-person days.
At home, if you can, use an air cleaner or crack open a window. And limit the amount of time your kids spend with elderly or vulnerable family members. Less exposure time means fewer virus particles shared.
– College Students
Are college students crazy and at risk of killing us all? No, they’re not exactly crazy. However, their decision-making skills are still developing until about age 25.
A young adult might decide to party unsafely because partying has no immediate downsides for them. If they catch coronavirus, it’s likely to be so mild that they don’t suffer – in fact, there’s a good chance they won’t know they have it. Does a family member then get infected? Well, who can say that the youth caused it? And does the collegian suffer heart problems later on? That’s far in the future and unlikely to worry them today.
So what are we all to do about college students in the family? Perhaps you believe that your young family member is unusually mature, and takes all the COVID precautions (as he or she no doubt tells you). But nevertheless, it wouldn’t hurt to keep some distance, and wear masks, for at least the first week or two when they come home to visit. And adding some fresh air in the house wouldn’t hurt either!
I hope these partial answers help you navigate through these difficult times with more confidence. Stay healthy, and always look on the bright side of life!
Image Credits:
– Infographic, COVID-19 Hospitalization and Death by Age, courtesy of CDC
– Bar chart (Ratio of Deaths to Hospitalizations) courtesy of StatNews.com
– Class and party images by cdc, Rebecca Zaal, Wendy Wei on pexels.com
– Beer garden party by juhel on openclipart.org

Hi Art,
Jacquie shared your comments. Nice to know you are well!
Mary Yamabe
Thanks, Mary. Hope all is great with you! & thx for looking at my blog! – Art